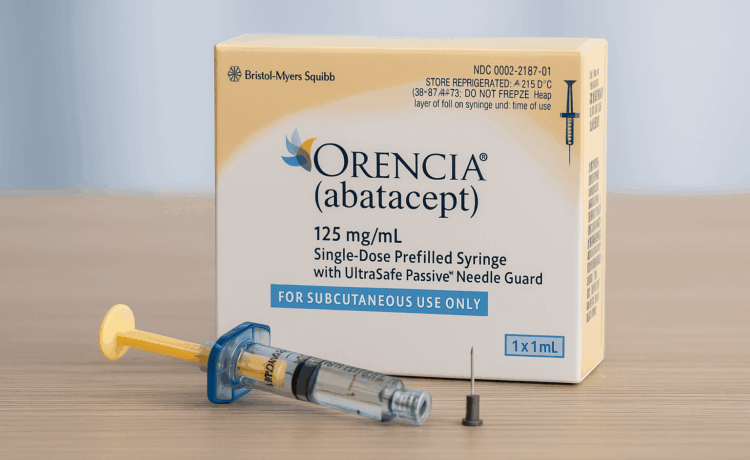
If you’ve been prescribed Orencia, the first thing you probably noticed is the price. The cost of Orencia shouldn’t keep you from accessing the treatment you need. At NeedyMeds, we connect people with programs that offer financial assistance, so they don’t have to choose between paying bills and managing their health. We believe access to medications like Orencia shouldn’t depend on your income or insurance plan. This article breaks down the true cost, what kind of help is available, and how to apply for it. Whether you’re looking for an Orencia coupon, a free medication program, or wondering how to […]