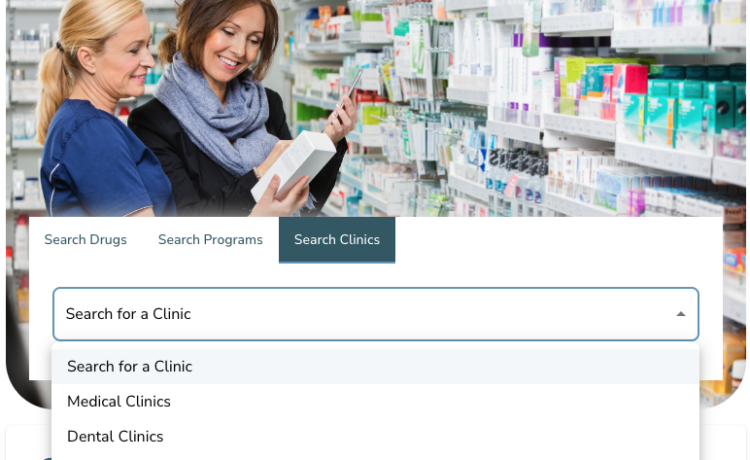
For many New Yorkers, accessing quality dental care at an affordable price can be challenging. In a previous post, we explored various options for budget-friendly dental services and how to search for them on our website. Here, we dive deeper into student-run clinics that provide dental services at affordable rates. Student dental clinics offer a great solution if you’re looking for budget-friendly dental services. These clinics provide services at free, low-cost, or sliding-scale rates, making dental care accessible to everyone. With help from certified experts, dental students offer care at a much lower cost than regular dental clinics. Common misconceptions […]