Last Updated on February 6, 2020
January is National Cervical Health Awareness Month in the United States. With all women being at risk for cervical cancer, it’s important to be mindful of the health risks, symptoms, and resources available to those in need. The Center for Disease Control (CDC) estimates 12,000 people are diagnosed with cervical cancer each year, and about 4,000 die from it annually.

The main cause of cervical cancer is human papillomavirus (HPV), a common virus that can be passed between people through sex or any genital skin-to-skin contact with someone who has the virus. HPV is so common that most people will have it at some point during their lives without ever developing symptoms. About 90% of cases are cleared naturally by the immune system within two years; however, there is no way of knowing which individuals will go on to develop health problems.
Some strains of HPV can cause warts around genitals or in one’s throat, while others can cause normal cells in the body to turn abnormal—possibly leading to cancer over time. Other factors that can increase your risk for cervical cancer are smoking, having HIV, using birth control pills for an extended time (five or more years), or giving birth to three or more children.
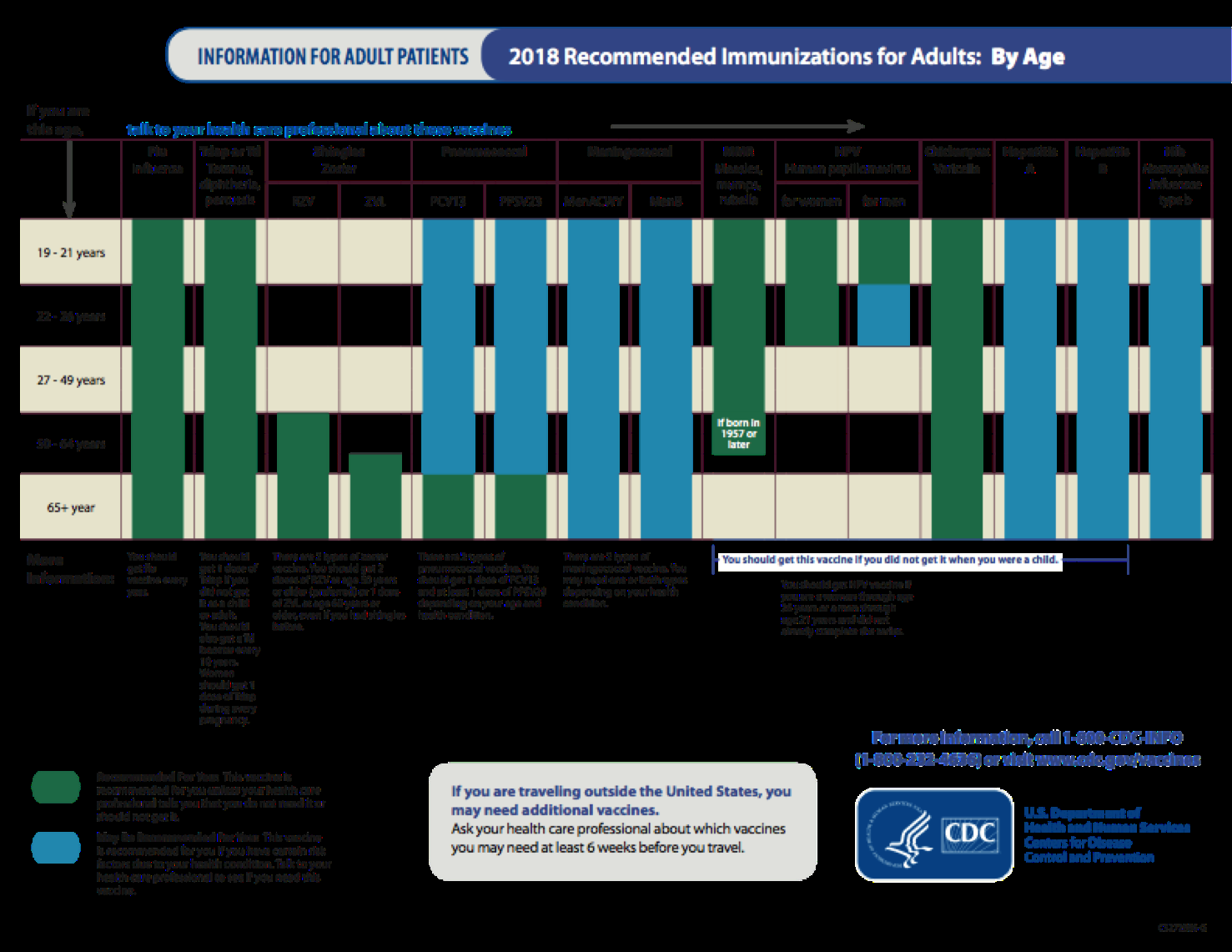
The most important thing one can do to prevent cervical cancer is to have regular screening tests starting at age 21. Regular Pap tests performed by a doctor are the main defense against cervical cancer. There are vaccines for HPV that can greatly decrease the chances of contracting the potentially malignant virus available to pre-teens and young adults. Safe sex practices can also reduce (but not eliminate) the risk of infection for both cervical cancer and HPV.
Cervical Health Awareness is important for more than just straight/cisgender women Transgender men are also at risk for cervical cancer if they still have a complete or partial cervix or if they have a history of cervical cancer, precancerous conditions, or HPV. Transgender people can experience additional barriers to screening such as discrimination and disrespect—one in five trans men report being refused health care based on their gender identity—which can cause many to postpone or avoid preventative care. Testosterone treatments common for trans men can also cause changes in the cervix that may appear precancerous, making the results of Pap tests difficult to interpret. Trans women who have undergone “bottom” surgery can also be at risk for cervical cancer depending on the type of surgery and the kind of tissue used to create one’s cervix. Transgender individuals should speak with their healthcare provider to see if a Pap test or comparable cancer screenings would be appropriate for them.
In a previous blog post, we featured the National Breast Cancer and Cervical Cancer Early Detection Program, a national government initiative that provides free or low-cost screenings for those who qualify and gives access to treatment through Medicaid for women diagnosed with cancer through the program. We had another blog covering Planned Parenthood’s many important services, including cervical cancer screenings. Planned Parenthood performed 378,692 Pap tests in 2013 alone. NeedyMeds has information on over 500 Planned Parenthood clinics; search your zip code for locations in your area.
Cervical Health Awareness is a nationally important matter. Women should be encouraged to get their well-woman visit with their doctor this year and be told of the resources available if they need help. Parents should know the HPV vaccine can also greatly decrease their children’s risk of contracting cervical cancer. For more resources, check our website Needymeds.org or call our toll-free helpline at 1-800-503-6897.