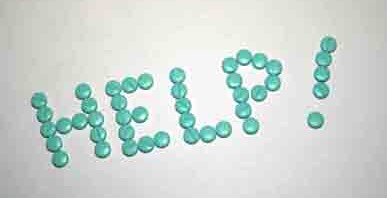
According to a September 2023 United States Census Bureau report, a staggering 26 million people are uninsured; per a January 2024 Forbes article, 43% of working-age adults are inadequately insured. Every month our helpline counselors answer 2,200+ calls from such vulnerable individuals seeking affordable healthcare. In their honor, this month, we’ve kicked off our Keep Us Talking fundraiser to ensure our helpline remains free of charge. This campaign isn’t just about a toll-free phone number; it’s about tearing down barriers that block the path to wellness: Limited finances Many individuals who utilize services like NeedyMeds are already facing financial hardship due […]