Black lives are being lost to COVID-19 at twice the rate of others. Black women are three to four times more likely to die from pregnancy-related causes compared white women. Black children are more than three times more likely to die after surgery than white children. Black people are 3.23 times more likely to die at the hands of the police than white people. The Black Lives Matter movement protests against the destructive devaluing of Black lives at the hands of law enforcement and other racially-motivated violence; it is equally clear that Black lives need to be more valued in terms of the healthcare they have access to and receive.
By nearly any measure, Black people suffer disproportionately in America. They face countless challenges to good health, among them food, transportation, and income. Healthcare services are often more expensive, with over 30% of medical expenses faced by BIPOC (Black, Indigenous, People of Color) being associated with health inequities. The stress of living life inescapably affected by racism has very real effects on a person’s physical and mental health.
Black people are less likely to use psychiatric medications or administer them to a child in their care, even when they have equal access. Aside from a lack of diversity, experts say that this is possibly due to a lack of cultural competence in the fields of healthcare and psychiatry. BIPOC are more likely to report a distrust of healthcare institutions, having historically been the subject of harmful experiments and forced sterilization.
BIPOC are under-represented in medical research, making the available information about their health sometimes less valuable or reliable. In dermatology, where images are critical for diagnoses, the lack of images of darker skin poses a significant barrier to proper treatment and medical education. Skin conditions can be subtler or harder to see in dark skin, and physicians who haven’t been adequately trained with such images are prone to misdiagnose people of color. Furthermore, experiencing discrimination and implicit bias from healthcare providers is associated with higher rates of psychiatric disorders, substance abuse, and suicide in patients of color.
As the COVID-19 pandemic continues to roll across the U.S., the virus has hit Black Americans exceptionally hard. Black people are more likely to live in poor neighborhoods, work at riskier occupations, and have more underlying health conditions and limited access to healthcare; but similar inequities even exist in Black communities with above-average wealth and healthcare access. BIPOC receive poorer quality care than white patients across all medical interventions and routine health services — even when insurance status, income, age, comorbid conditions, and symptom expression were equal. Differences even exist between Black and white patients in the length of wait time for appointments and the ability to schedule follow-up appointments. This can result in delayed healthcare — which leads to higher costs and poorer health outcomes for illnesses, including COVID-19.
Starting from a young age Black children are more likely to be disciplined or receive harsher punishments, though no studies have proven that Black students misbehave at higher rates. Minor transgressions, such as cannabis possession (even in states where it’s been legalized), are aggressively enforced in communities of color with ramifications that can lead to a lifetime of lost opportunities for adolescent BIPOC that white people rarely face, notwithstanding comparable usage rates.
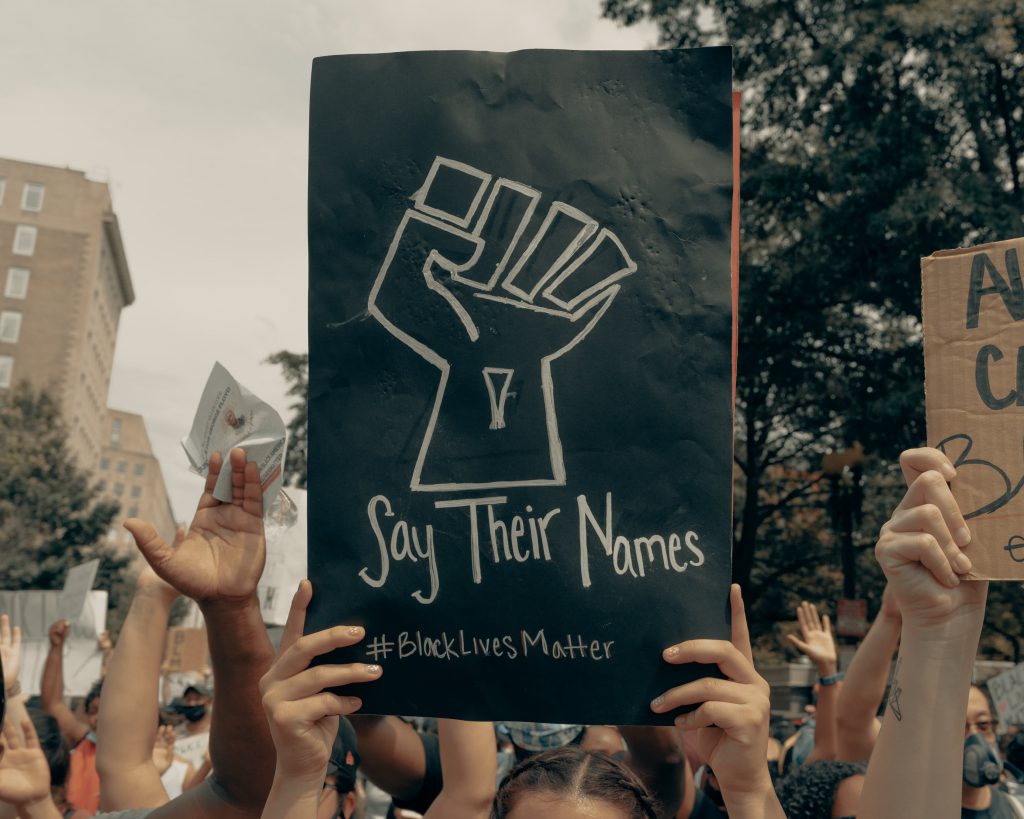
People of color experience inordinate violence by law enforcement, which greatly affects the public health of their communities. Police interactions perceived as unfair, discriminatory, or intrusive are associated with adverse mental health outcomes including symptoms of anxiety, depression, and post-traumatic stress disorder (PTSD). Violent policing, criminalization, and incarceration are all threats to health. Even wearing a mask during the ongoing pandemic can put Black people at risk of being harassed or profiled. Racism and police brutality have been declared serious public health crises by health groups such as the American Medical Association (AMA), American Nurses Association (ANA), National Nurses United (NNU), and the American Psychiatric Association (APA).
Black people of all ages are frequently the target of anti-Black vigilantism or law enforcement weaponized against them for being “suspicious.” Innocent Black lives can even be lost when police serve a no-knock warrant to the wrong address for a suspect who was already in custody. The systemic lack of accountability for these senseless deaths can make whole communities feel helpless or angry in the face of injustice and weighs heavy on the mental health of the entire nation.
Negative experiences with law enforcement can make communities less likely to report crimes or missing persons; worsened by data showing that missing white children receive far more media coverage than missing BIPOC children despite higher rates of missing children among communities of color. Crimes against Black people can also go under-investigated. Hanging deaths of BIPOC are often dismissed as suicide, reminding some of the dark roots of lynchings going unpunished in America.

Intersectionality can exacerbate a person’s experience of intolerance. Intersectionality is the interconnected nature of social categorizations such as race, class, sexuality, and gender identity/expression as they apply to an individual that overlap with interdependent systems of discrimination or disadvantage. BIPOC who are LGBTQIA (lesbian, gay, bisexual, transgender, queer, intersex, and asexual) can experience body dysmorphia, physical or emotional abuse, or feeling unsafe at school or work in concert with the detriments of systemic racism. The Trump administration has rolled back protections of LGBTQIA people to make it easier for them to be discriminated against at the workplace, at school, in healthcare, housing, and public life. Trump has even attacked anti-segregation rules with divisive and racist alarmism.
Studies have shown that long-term discrimination can lead to a disruption in the stress hormone cortisol, leaving people with less biological energy and more fatigue. That type of chronic sustained stress contributes to health conditions like diabetes, obesity, and depression. It can all take a significant toll on a person’s mental health. The prevalence of news media depicting police violence and viral videos of racial profilings can have PTSD-like effects on young BIPOC — to say nothing of a person’s individual experiences of racism, isolation, being silenced or stripped from their sense of belonging.
Mental health care can be vital for anyone, especially those affected by racism and discrimination. When meeting with a provider, it can be helpful to ask questions to get a sense of their level of cultural sensitivity. Providers expect and welcome questions from the patient since this helps them better understand what is important in their tre11atment. Some questions to consider asking are:
- Have you treated other BIPOC?
- Have you received training in cultural competence or BIPOC mental health?
- How do you see our cultural backgrounds influencing our communication and my treatment?
Your mental health provider will play an important role in your treatment, so make sure you can work with this person and that you communicate well together. Mention your beliefs, experiences, values, and cultural characteristics. Make sure that they understand them so that they can be considered in the course of your treatment.
NeedyMeds has information for over 6,000 free, low-cost, or sliding-scale clinics throughout the country that offer counseling or mental health services. Search your ZIP Code for mental health clinics near you, or call our toll-free helpline for information at 1-800-503-6897 (open Monday through Friday, 9am to 5pm ET).
We encourage everyone to educate themselves, strive to understand the difficulties and experiences people around us live with, and to replace stigma and bias with hope and support. If you or someone you know is suffering in these trying times, it is important to know that no one is alone in their struggle. Call for assistance, whether help is needed immediately or long-term.
Samaritans 24/7 Crisis Services via call or text: (877) 870-HOPE (4673)
The Steve Fund Crisis Text Line (crisis support for people of color): Text STEVE to 741741
The Trevor Project (LGBTQIA crisis support): 1-866-488-7386 or Text “Trevor” to 1-202-304-1200
Trans Lifeline (transgender crisis support): (877) 565-8860
For George Floyd, Breonna Taylor, Ahmaud Arbery, Elijah McClain;
For “those who burned, those still aflame, and the countless unnamed.”
Rest in power.
Black Lives Matter.
(quotation from the poem Coded Language by Saul Williams)