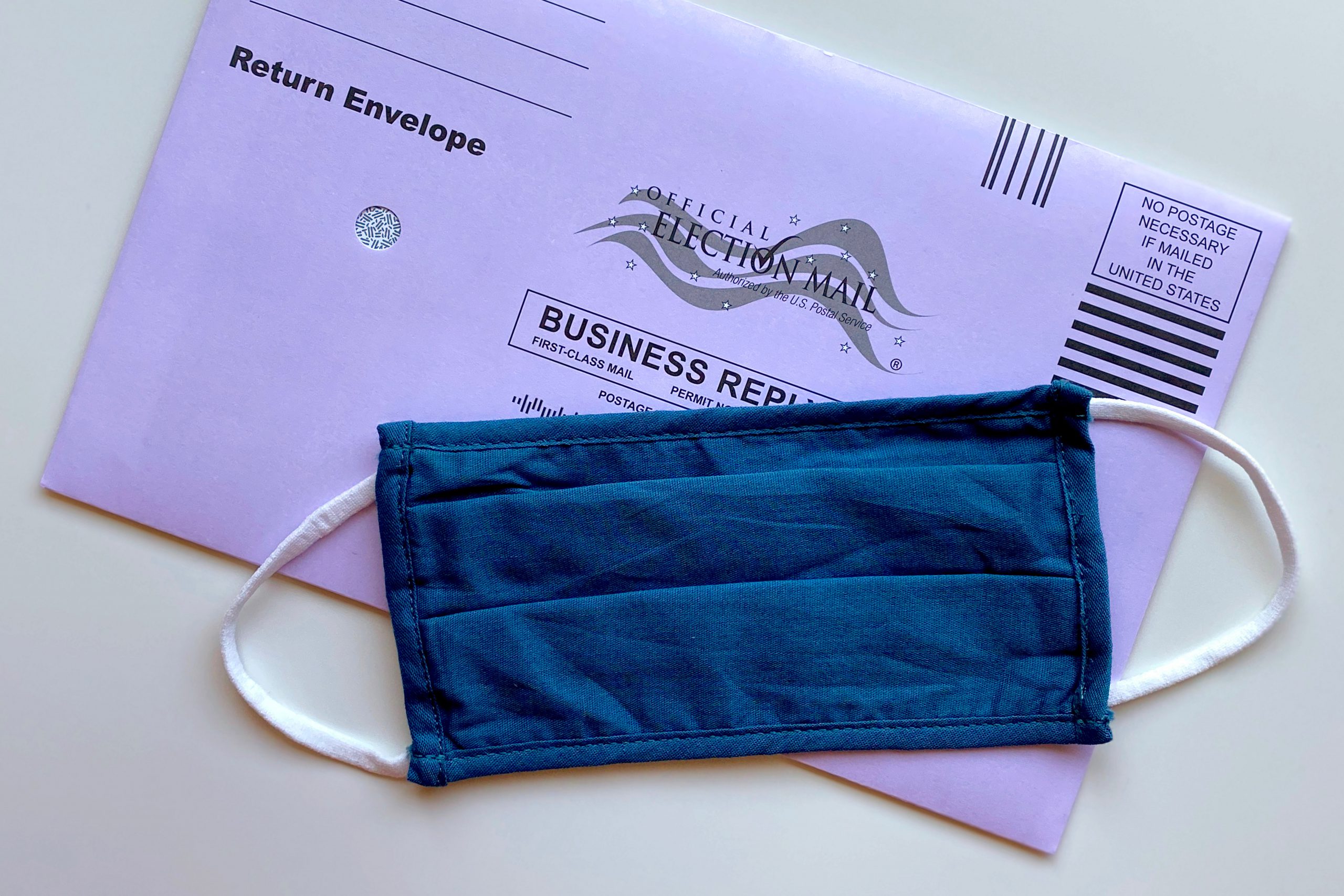
We are getting further away from Election Day in the U.S. and getting closer to 2021 when many of the changes voted on and passed will begin to take effect. Americans voted for much more than president that will impact our nation’s healthcare this past November. Several states voted to legalize or decriminalize cannabis (aka marijuana), therapeutic use of psychedelic mushrooms, and Oregon voters approved a measure that decriminalizes small possession amounts of all illicit drugs. Five states — Arizona, New Jersey, South Dakota, Montana and Mississippi — voted to legalize some form of cannabis use. Despite being a […]