Having health insurance is vital to one’s health and financial well-being in the United States. Out-of-pocket medical expenses are the leading cause of personal bankruptcy. Even with new laws such as the Affordable Care Act (ACA)—aka “Obamacare”—11.7% of Americans remain uninsured. Analysts have only recently been able to examine the data of uninsured rates prior to ACA’s implementation to now. WalletHub released the stats for all 50 states and Washington DC and ranked each by their current uninsured rate; Massachusetts is ranked highest with only 3.28% uninsured, and Texas is ranked last with 19.06%. In numbers, even the last-ranked […]
Category: Affordable Care Act

Medication Costs on the Rise
Last month, we posted a blog about how many Americans are spending more than $50,000 or even $100,000 a year on medications—more people than ever before. The information included insured Americans and found that insurance covered an average of 97% of prescription costs for those spending at least $50,000. At NeedyMeds, there are many assistance programs for those who are in need. However, even with new laws and regulations there are those stuck in between. There are patients in America that make too much money to qualify for assistance but still not enough to pay all their medical bills. […]
Affordable Care Act Helps Americans Ages 50-64
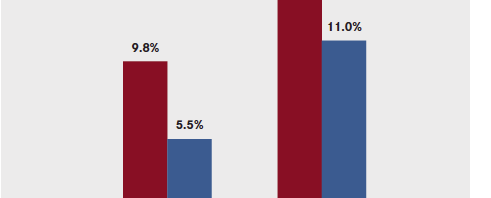
In the past five years since the passage of the Affordable Care Act (ACA), there have been strong supporters and fierce opponents. No matter what side of the ACA one falls, it’s hard to deny the positive results it has had in some people’s lives. Since 2013, uninsured rate dropped by 31% among Americans ages 50-64. Elderly Americans are among the most underserved populations in the country, and are at risk of struggling with poverty and disparity in health care. The ACA expanded access to health insurance coverage to 50- to 64-year-olds through several provisions, including expanding eligibility for […]
All About Medicaid
Here at NeedyMeds we regularly refer people to their state’s Medicaid program, and in today’s blog post we are going to explain exactly what Medicaid is and how it functions. Are you currently enrolled in Medicaid? Share your experience with us in the comments section. How is it Financed? Medicaid, sometimes called Medical Assistance, is a joint federal and state entitlement program for people with limited income that helps to pay for medical costs. It receives a combination of funding from both the state and federal government. The amount paid to each state by the federal government, also known […]

The Affordable Care Act and the Future of Assistance Programs
We’ve been getting a lot of questions from our readers about how the resources we list on our website, especially the pharmaceutical patient assistance programs, will be affected by the Affordable Care Act. While we are still far away from having all the answers, we do have some additional information we can provide you after attending a recent PAP Conference. The overarching consensus is that PAPs will continue to exist to help those in need that fall into the gaps. Here is an overview of what we learned at the CBI PAP 2014 Conference, held in Baltimore on March 6-7. […]
