Last Updated on May 25, 2023
The Federal Government declared a COVID-19 public health emergency in January of 2020 and decreed many changes in healthcare and healthcare insurance to help people better cope with the pandemic. The Coronavirus Preparedness and Response Supplemental Appropriations Act of 2020 provided $6.7 billion for the federal and state governments to respond to the COVID epidemic in the United States. An additional $1.6 billion was included to contribute to the international response.
The majority of the funds were used to control the virus in the form of research into treatment and prevention measures; keeping track of all aspects of the pandemic (evolving variants, the number and locations of cases, hospitalizations, and deaths); emergency use authorizations for COVID vaccinations and treatments; and paying for COVID-19 preventive measures, testing, treatment, and vaccinations.
Funding was made available to help defer medical costs for certain individuals, such as allowing those on Medicare to access certain telehealth services, a 20% increase in Medicare reimbursements for hospitals to treat COVID-19 patients, requiring Medicare Advantage plans to charge in-network prices for care provided at out-of-network facilities, and prohibiting states that received enhanced Medicaid funding to drop individuals from Medicaid (Medicaid continuous enrollment provisions). Households and college students participating in the Supplemental Nutrition Assistance Program (SNAP) could get emergency allotments to purchase necessary food. The Appropriations Act also provided emergency financial support for any small business affected by the pandemic. Finally, the legislation provided funding for regulation and oversight of the response to COVID-19.
Other non-economic measures that were taken included:
- Giving healthcare providers expanded telehealth access and benefits, including allowing Medicare beneficiaries to remain in their homes for telehealth visits, providers to deliver telehealth services by smartphone, and to bill televisits the same as office visits.
- A waiver allowing the renewal of a prescription for controlled substances, including opioids, with only televisit rather than an in-person visit.
- Waivers for staffing flexibilities, such as allowing nurse anesthetists, as well as NPs in some settings, to work without physician supervision;
- Allowing physicians’ whose privileges expired or new physicians without full approval to practice at hospitals to alleviate workforce shortages;
- Giving hospitals extended timelines to complete medical records and waivers of requirements for utilization review to assure that hospitals are compliant with certain HIPAA requirements;
- Authorizing pharmacists and pharmacy technicians to order and administer COVID-19 tests, vaccines, and treatments for patients as young as three; and
- Other relaxations of certain regulations for hospitals and healthcare providers.
SNAP emergency allotments and the Medicaid continuous enrollment provisions have already lapsed and the remainder of the COVID public health emergency provisions ended on May 11. This corresponds with the World Health Organization’s May 5th declaration that the COVID global health emergency has ended.
Since COVID-19 is still with us, the end of the public health emergency will have a significant impact on COVID-related healthcare. These changes will result in higher costs for treatment, vaccination, and health insurance and more difficulty accessing care, such as telehealth and free or low cost clinics.

The major impact will be the cost of COVID-19 testing, medications and vaccines, especially for those without healthcare insurance. The effect may not be seen immediately, but will slowly emerge as current supplies run out. For those on Medicaid, COVID-19 testing, vaccines, treatments, and some medical devices will be covered for a year. COVID-19 vaccines are expected to be covered by Medicare and some community programs.
As with most conditions, insurance will probably pay for at least some or all of the cost of COVID treatments and vaccinations, and COVID tests ordered by healthcare providers and done at commercial laboratories. Home testing will probably not be covered, although there may be many places to get them at no cost, such as various community testing centers.
Overall, insurance premiums and out-of-pocket spending may be higher if the treatment and testing costs are substantial and if hospitals try to make up for lost Medicare payments for treating patients with COVID infections, renewed problems with staffing, and the need to increase efforts to meet HIPAA requirements by increasing fees. Out-of-pocket spending will be higher for those with Medicare Advantage plans since the plans will again be able to charge out-of-network prices for unauthorized visits.
The Food and Drug Administration (FDA) will continue to authorize some COVID-19 vaccines and antiviral drugs, like Paxlovid, for emergency use, have tests, treatments, and vaccines available for emergency use when criteria for issuance are met, and streamline the availability of new COVID-19 drugs. The federal government will continue to fund research to develop new COVID vaccinations and treatments.
Millions of families currently on Medicaid are at risk for losing their healthcare if they no longer qualify after their states redetermine their eligibility requirements. The Special Enrollment Period for the Affordable Care Act (ACA) has been extended to allow these families to obtain health insurance through the ACA marketplace. They also extended the deadlines for healthcare insurance claims and appeals and COBRA insurance applications, although the length of extension is not known.
Telehealth visits will still be allowed for those with Medicare, Medicaid, and private insurance depending on the terms of individual policies. The healthcare providers expanded telehealth access and benefits have been extended through the end of 2024. It is likely in the long-term that healthcare providers will have to bill less for telehealth visits.
The DEA has extended virtual renewals of controlled substances such as opioids for pain and stimulants for ADHD for another 6 months, after which the requirement for in-person prescribing will resume. Methadone for opioid use disorder treatment will remain available by virtual visits for one year and buprenorphine for opioid use disorder treatment will remain available by virtual visits indefinitely.

Many of the waivers offered to hospitals and healthcare providers — such as reduced supervision of providers that are not fully trained, relaxed HIPAA oversight, reduced regulation, and exemptions from some sanctions — will expire, while some that have resulted in more effective patient care will not. Hospitals and healthcare providers will return to their previous billing practices. They will lose the 20% increase in Medicare payments and not be able to bill more for COVID related services and telehealth visits.
Many pandemic-controlling measures have stopped.
- Most federal COVID-19 vaccine mandates have been lifted for federal employees and contractors.
- There are no longer COVID vaccine requirements and other COVID restrictions for international travelers.
- The CDC has stopped tracking some COVID statistics, including the number of COVID infections, community levels of COVID, and the number of positive COVID tests. They will still track COVID infections by testing wastewater and monitoring hospital admissions for coronavirus, but overall this will make it harder to immediately identify any new surges in COVID infections.
- Title 42 immigration restrictions have stopped, but the Biden administration has created a plan to restrict asylum that can be used to deport migrants who cross the U.S.-Mexico border without a previous request for asylum.
Emergency Use Authorizations for COVID tests, vaccines, medications, and certain medical devices and many programs will be phased out over time.
| June 9, 2023 | College Student SNAP benefits. |
| July 10, 2023 | Medicaid Section 1115 Emergency Waivers, if not already ended
Extended deadlines for healthcare insurance claims and appeals and applying and paying for healthcare insurance through COBRA or the Affordable Care Act marketplace |
| August 9, 2023 | FEMA Public Assistance for demobilization, disposition, disposal cost for COVID-related disasters |
| September 30, 2023 | Medicare New COVID-19 Treatments Add-on Payments |
| November 11, 2023 | Medicaid Section 1915(c) Appendix K Waivers for HCBS
Telemedicine flexibilities for prescribing of controlled substances (with a 12-month extension for provider-patient telemedicine relationships established by Nov. 11, 2023) The National Health Service Corps program to hire healthcare providers willing to work in the country’s underserved area in exchange for forgiving school debts. |
| December 31, 2023 | The enhanced federal matching payments tied to Medicaid continuous enrollment provision |
| April 30, 2024 | Hospital COVID-19 data reporting requirements |
| September 30, 2024 | The requirement that at-home COVID-19 tests be provided for free and COVID-19 PCR/provider-ordered tests be done at no charge to Medicaid enrollees
The requirement that treatments provided with no cost sharing to Medicaid enrollees The 100% federal Medicaid matching payments for vaccine administration |
| November 11, 2024 | Telemedicine flexibilities for prescribing controlled substances for provider-patient telemedicine relationships established by November 11, 2023 |
| December 31, 2024 | Expanded telehealth coverage under traditional Medicare,
Liability protections for pharmacists, pharmacy interns & techs to administer COVID-19 and flu vaccines to those ages three and older and to administer COVID-tests (although this may be extended indefinitely) Liability protections for COVID-19 countermeasures provided through Federal agreements or directly conducted by the US government PREP Act |
| September 30, 2025 | FEMA COVID-19 funeral assistance |
Although the public health emergency has been declared over, COVID-19 is still a pandemic and will continue to have an effect on our lives and healthcare for a long time. Most of the effects will be financial in the form of higher costs for healthcare, healthcare insurance, and even food for some. Unfortunately, a lot of the expired measures will make it easier for COVID to become a significant problem again if we are not vigilant in keeping track of COVID outbreaks, emerging variants, and using preventative measures should the situation arise in our community.
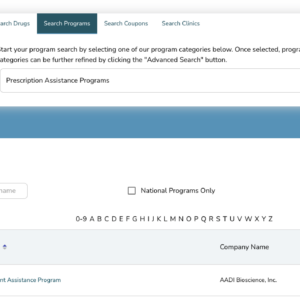
If you or your family is in need of care but lack the means to find affordable treatment, NeedyMeds has a database of over 18,000 free, low-cost, or sliding scale clinics across the United States and its territories. Search your ZIP code for clinics in your area to find free or low-cost medical attention. You can also use Vaccines.gov to find COVID-19 vaccinations in your area. NeedyMeds lists over 100 nationwide resources for those who have been impacted by COVID-19. For more help finding information, call our toll-free helpline Monday-Friday 9am-5pm Eastern Time at 1-800-503-6897.