Last Updated on September 2, 2020
The effects COVID-19 has had on healthcare have been a significant part of nearly every article written here since March. The last time we looked into the costs associated with coronavirus infections, things were very different. We didn’t know what the summer would look like or how schools would reopen. Daily briefings from the White House were still happening.
The first U.S. case of COVID-19 was discovered in late January. By the end of February, there were 24 cases and one American death. In the first few weeks of the outbreak testing was very limited, sometimes as few as 300 for an entire state. It then took time for health officials to realize that the tests they received were flawed, lacking critical components, and delivering faulty results.
In late February, a Seattle team researching the flu found they could test for the SARS-CoV-2 coronavirus that causes COVID-19, but were running into bureaucratic red tape. When the doctors decided to circumvent the regulations in the interest of public health and began finding positive results, they were explicitly told by federal officials to stop testing in an attempt to keep the official numbers low.
Through March and April the number of confirmed cases doubled every few days, reaching a million shortly after the daily White House briefings stopped in late April. One day in early May saw 5000 deaths. The U.S. reached the 2 million cases milestone in early June, and then doubled it to 4 million in six weeks.
Deaths have ranged from 500-3000 every day for months. At the time of publishing, the United States is leading the world with over 6 million cases and nearly 185,000 dead from COVID-19. The U.S. contains 4% of the world’s population, but upwards of 20% of global cases and deaths from the pandemic. COVID-19 is now the third leading cause of death in the United States, only surpassed by heart disease and cancer. These numbers do not include patients who died as a result of fewer available resources from the strained healthcare system.
The pandemic affects every aspect of American life:
- 42% of Americans now work from home full-time;
- a third of working-age adults have been unable to work (and have since lost their federal emergency aid added to unemployment assistance);
- essential workers such as those in healthcare, postal service, food production/shipment, grocery sales, garbage collection, fire/rescue, etc have continued to work often without appropriate personal protective equipment (PPE) or hazard compensation;
- students of all ages have switched to online learning or had to discontinue their education;
- patients have been subject to restrictions on hospital admissions, visitation, and out-patient appointments;
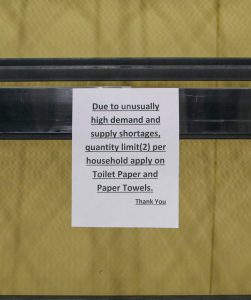
- there have been shortages for disposable paper products, soap/sanitizer, PPE, testing equipment, and other necessary goods.
This is nowhere near an exhaustive list. Every interaction can come with risk of coronavirus infection — all while dangerous misinformation and conspiracies have been prevalent and the realities of the pandemic have been minimized for months. After a summer of canceled events and travel restrictions both internationally and domestic, schools are now facing political pressure to open for in-person learning despite the many health safety concerns for teachers, students, and their families.
Racism is another unfortunate factor surrounding COVID-19. The novel coronavirus causing the disease was first detected in Wuhan, China. Despite the scientific classifications, some people — including President Trump and members of his administration — have continually attributed the disease to a name with overtly racist connotations: “Chinese virus.” Attaching the virus to an ethnicity has caused Asian-Americans to become targets of racism and xenophobia, making them subject to hostile remarks and physical assault. This racial profiling and targeting stems from the false notions that East Asians are to blame for the emergence of COVID-19 and/or are viral carriers by virtue of their ethnicity. Normalizing the association between the coronavirus and those of Asian descent only causes further divide at a time when fear and confusion surround the facts. There are now more than 65 times the confirmed cases of COVID-19 in the United States than were detected in China and over 38 times as many deaths.
Dr. Anthony Fauci became somewhat a public figure as director of the National Institute of Allergy and Infectious Diseases during his tenure as a central member of the White House Coronavirus Task Force. He has expressed frustration at the flow of misinformation and racism coming from the president. Experts and health officials join him in warning against following the president’s optimism surrounding potential treatments so early in researching them.
Americans are continuing to face unexpected costs from coronavirus-related healthcare. Early in the pandemic, a family that had traveled back to the U.S. from Wuhan, China faced government-mandated quarantine only to be told they owe $3900 for their involuntary isolation. A patient who hadn’t met the prerequisites for being screened for coronavirus received a $2777 bill after a battery of tests to rule out other diagnoses. An uninsured lymphoma patient was charged nearly $35,000 after three emergency room visits over the course of a week, and a diagnosis with COVID-19 three days later.
President Trump claimed that insurers had agreed to cover the costs of coronavirus treatment, though that was unfortunately not true. Insurance companies had agreed to cover the costs of testing for coronavirus, but not copays for treatment. The Trump administration has since weakened insurance companies’ commitments, allowing them to determine if a test is “medically appropriate” before waiving costs for patients getting screened for COVID-19. For the millions of new and existing uninsured and underinsured Americans, there are no guarantees for coverage of costs upwards of $75,000. Several states offered their uninsured residents another opportunity to sign up for a health plan this year as they seek new ways to fight the novel coronavirus pandemic, though the Trump administration declined to reopen Obamacare enrollment.
The ultimate goal of protecting the world’s population from the COVID-19 pandemic is to develop a vaccine against the novel coronavirus. Dr. Fauci has said the SARS-CoV-2 coronavirus “might keep coming back” year after year but noted, “We’ll be much better prepared. We’ll likely have interventions, but the ultimate game-changer in this will be a vaccine.” The World Health Organization (WHO) has launched an initiative to fast-track the development and scale-up of COVID-19 vaccines and make them available to nations who need them the most, while the Trump administration has said that there will be “no guarantee” that every American will be able to afford the COVID-19 vaccine once it is developed. Only when everyone can reliably be immunized against coronavirus could the world declare COVID-19 pandemic over.
More than 170 teams of researchers are racing to develop a safe and effective coronavirus vaccine, with only a few dozen progressing past pre-clinical trials. Vaccines normally require years of testing and additional time to produce at the necessary scale, but scientists are hoping to develop a coronavirus vaccine within 12 to 18 months. Some scientists, however, have concern over political pressure prematurely forcing a vaccine into production before this November’s election.
The circumstances and information surrounding COVID-19 are constantly evolving. We at NeedyMeds will continue to keep our users apprised of new information as it becomes available as well as counter misinformation in the interest of keeping our readers safe.
If you are presenting symptoms and think you may have contracted COVID-19, call your healthcare provider or local healthcare facility. Based on your symptoms and exposure, they will decide if you need to be evaluated in person and may confer with state authorities about where and how to do the testing. They will give you instructions on how to arrive in a way that limits exposure. Medical facilities and doctors’ offices ask that everyone call ahead so they can make arrangements to protect others when people come in for testing. There may still be a shortage of tests. In the meantime, if you think you might have the coronavirus, assume you have it and self-isolate. Take all measures to prevent spread — wearing a mask and social distancing in particular.
The NeedyMeds website has a database of 119 nationwide resources for those who have been impacted by COVID-19. We also have listings for over 18,000 free, low cost, or sliding scale clinics for those concerned about the costs of healthcare. Search your ZIP code for clinics in your area to find free or low-cost medical attention. Remember to call first if you are seeking information about availability of COVID-19 testing. The free NeedyMeds Drug Discount Card can be used by anyone to help save money on their prescribed medication — even over-the-counter medicine if prescribed by a doctor. The card is available physically via mail, in a printable form, or as a smartphone app for Apple and Android devices. For more help finding information, call our toll-free helpline Monday-Friday 9am-5pm Eastern Time at 1-800-503-6897.