Last Updated on January 30, 2020
This blog post originally appeared on Zaggocare.org
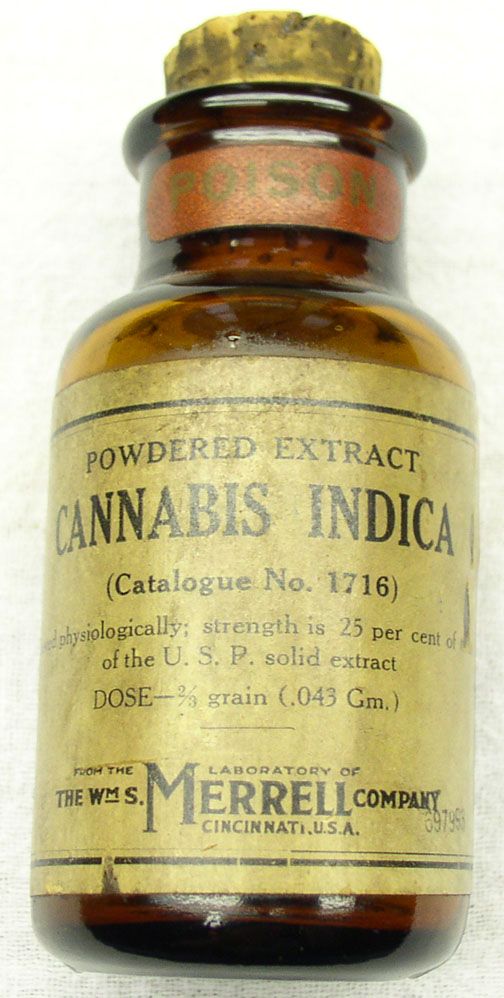
 Medications save lives and make life more bearable for millions of people. No doubt about it. But medications can also cause harm. Logically, the more medications a patient takes, the higher the risk of side effects and dangerous interactions between medications. Did you know many patients take inappropriate or unnecessary medications? Unfortunately, over-prescribing is a widespread, dangerous problem in the US, especially for older patients (categorized as those 65+ years old). Why do doctors prescribe too many medications? What harm does it cause? And what can patients do?
Medications save lives and make life more bearable for millions of people. No doubt about it. But medications can also cause harm. Logically, the more medications a patient takes, the higher the risk of side effects and dangerous interactions between medications. Did you know many patients take inappropriate or unnecessary medications? Unfortunately, over-prescribing is a widespread, dangerous problem in the US, especially for older patients (categorized as those 65+ years old). Why do doctors prescribe too many medications? What harm does it cause? And what can patients do?
An extensive report by the Lown Institute examines the impact of over-prescribing in older patients. Their report states that the US “is in the grips of an unseen epidemic of harm from the excessive prescribing of medications.” This important, often overlooked issue may impact your health, or the health of a loved one.
What are the dangers associated with medications?
Although medications are designed to help patients, they can also cause health issues. All medications have side effects. Some are potentially serious, while others are minor. But it’s important to understand that all medications carry some degree of risk. There are two major issues of concern – side effects and adverse drug reactions.
Adverse drug reactions (ADR) involve an unexpected or dangerous reaction to a medication. You can develop an ADR after one dose of medication, from prolonged use of a drug, or from a negative interaction between 2 or more medications.
The more medications you take, the higher your risk of problems, an issue called medication overload.
What is Medication Overload?
According to the Lown Institute report, medication overload is “the use of multiple medications for which the harm to the patient outweighs the benefit. There is no strict cutoff for when the number of medications becomes harmful, but the greater number of medications a person is taking, the greater their likelihood of experiencing harm, including serious adverse drug events.”
It’s as serious as the opioid crisis!
The Lown Institute reports that “medication overload is causing widespread yet unseen harm to our parents and our grandparents. It is every bit as serious as the opioid crisis, yet its scope remains invisible to many patients and health care professionals.”
How many medications are older Americans taking?
Older Americans, as a group, are taking a lot of medication:
- More than 40% of older adults take 5 or more prescription medications a day, an increase of 300% over the past two decades!
- Almost 20% of older adults take at least ten medications.
What is the impact of medication overload?
Health issues from medication overload can range from mild to life threatening. And the economic ramifications are staggering.
The Lown Institute report found that in 2018, in the US:
- Medication issues led older adults to seek medical care nearly 5 million times.
- Every day approximately 750 older people end up hospitalized due to medications, for a total of over 250,000 hospitalized patients/year.
- These hospitalizations cost an estimated $3.8 billion.
Over the last decade:
- There were over 35 million cases of older people seeking medical treatment for adverse drug events.
- Medication issues led to 2 million hospital admissions.
 The Lown Institute estimates that if changes are not made, in the next 10 years medication overload will lead to premature deaths for 150,000 older Americans and reduce the quality of life for millions more. Furthermore, the report estimates that reducing inappropriate or unnecessary medications could save as much as $62 billion over the next 10 years. And that’s only for money saved by avoiding unnecessary hospitalization for older adults. Certainly, there could be huge additional savings by keeping all patients, of all ages, healthier by reducing medication overload across the board.
The Lown Institute estimates that if changes are not made, in the next 10 years medication overload will lead to premature deaths for 150,000 older Americans and reduce the quality of life for millions more. Furthermore, the report estimates that reducing inappropriate or unnecessary medications could save as much as $62 billion over the next 10 years. And that’s only for money saved by avoiding unnecessary hospitalization for older adults. Certainly, there could be huge additional savings by keeping all patients, of all ages, healthier by reducing medication overload across the board.
What factors lead to medication overload?
Although many factors influence medication overload, the Lown Institute report identifies 3 overarching issues:
Culture of Prescribing
The culture of prescribing is shifting. Doctors and patients feel the need to “do something” to improve patient health. Ads for prescription medications encourage patients to seek medications for improved happiness and health. The practice of medicine is fast paced, with doctors often seeing patients in time-limited slots. Additionally, we have adopted a medical approach to normal aging. All these factors have led to a shared expectation among doctors and patients that there is a “pill for every ill.”
Information & Knowledge Gaps
Doctors and other clinicians, as well as patients, don’t always have the critical information and skills they need to evaluate the circumstances and make informed decisions regarding medications.
Fragmented Care
There is a widespread lack of communication among a patient’s various doctors and other healthcare providers. As a result, patients can suffer. One common scenario: one doctor writes prescriptions for what seems like a new health condition but is actually a side effect from another medication prescribed by another doctor. This practice, referred to as “prescribing cascade”, can lead to a cycle of debilitating health and even death.
A story of a devastating prescription cascade.
The story below illustrates how medication overload, due to a prescription cascade, killed Joe Esposito.
Joe Esposito was remarkably healthy, running half-marathons in his 50s. Unfortunately, a slew of medications left him on the brink of death in just a few years. Joe suffered from mild to moderate Crohn’s disease, an annoying, but rarely fatal condition. Through the process of seeking treatment, his list of medications cascaded from 1 to 6 to 20. Unfortunately, each new medication led to new side effects.
The cascade started with steroids for Crohn’s leading to bone loss and anal fistulas. Doctors prescribed antibiotics for the fistulas, which led to peripheral neuropathy in his feet. Since the pain made it difficult to sleep, doctors gave him benzodiazepines and Ambien for sleep, along with Lyrica for the nerve damage and Tramadol for the pain. And then he developed severe diarrhea from several of the medications. Doctors gave him medications for the diarrhea, including opium drops. Furthermore, drugs weakened his kidneys, which in turn raised his blood pressure, so doctors prescribed 4 blood pressure medications. And, doctors gave him an experimental anti-inflammatory drug which led to pericardial tuberculosis, which almost killed him.
At the end of his life, Joe took over 20 different medications each day, but not one of his doctors considered this a problem worth addressing. Moreover, no one stopped to consider that all of these medications caused his symptoms, not the Crohn’s disease.
What are doctors, hospitals and the government doing about this?
 Not as much as we would hope and deserve! Although some doctors strive to minimize medication overload among their patients, there is no professional group, public organization, or government agency to date has formally taken responsibility for addressing this problem. The Lown Institute “calls for the development of a national strategy to address medication overload and help older people avoid its devastating effects on the quality and length of their lives.” Hopefully government agencies, non-profit organizations, hospitals and doctors will unite to address this serious issue.
Not as much as we would hope and deserve! Although some doctors strive to minimize medication overload among their patients, there is no professional group, public organization, or government agency to date has formally taken responsibility for addressing this problem. The Lown Institute “calls for the development of a national strategy to address medication overload and help older people avoid its devastating effects on the quality and length of their lives.” Hopefully government agencies, non-profit organizations, hospitals and doctors will unite to address this serious issue.
What can you do?
While we wait for a national strategy to reduce medication overload, there are some steps you can take to reduce your own risk of medication issues. I suggest the following:
- Carry a list of all medications with you – on your phone, or in your wallet – and keep this list updated as you add and remove medications. Be sure to include over-the-counter medications.
- Make sure all your doctors have an accurate list of all your medications, including over-the-counter. At every appointment, your doctor (or a staff member) should ask you to confirm your medications. Listen carefully, check the doctor’s list against your own list, and make any corrections needed. Do NOT assume that each one of your doctors has access to your medication list via your Electronic Health Records (EHR). Many EHRs do not connect to each other.
- When a doctor recommends a new medication, ask these questions:
- Is the medication absolutely necessary?
- What will happen if you don’t take it?
- Is there a chance your doctor is giving you this new medication to treat side effects from other medications you are taking? If so, what other options do you have?
- Are there lifestyle changes you can try first?
- Is the doctor giving you the smallest dose possible for your condition?
- Will this new medication interact negatively with other medications you’re already taking?
- Exactly how and when should you take it?
- Ask each doctor on your medical team if you can eliminate, or reduce, any of the medications you take.
- Don’t push your doctor to prescribe medication. Push aside the temptation to get “a pill for every ill”. And just because you saw an ad for a medication on TV, or a friend told you how much it helps her, it doesn’t mean it’s right for you.
About Zaggo:
 Roberta Carson started Zaggo, a non-profit organization to help patients and family caregivers manage illnesses and injuries, after her experience as caregiver for her teenage son Zachary during his 27-month battle with terminal brain cancer. Roberta realized patients and families urgently need practical, easy-to-use information and tools. Zaggo’s mission is to provide patients and families with the educational information, tools, and resources they need to become empowered, engaged, effective members of their medical teams for the best possible care. With an easy-to-use guide book and organizational tools, the ZaggoCare System is the only product to offer the comprehensive advice and tools needed to help patients and caregivers manage illness or injury. As a charitable organization, 100% of the profits from the sale of ZaggoCare are donated to innovative brain tumor research in memory of Zachary.
Roberta Carson started Zaggo, a non-profit organization to help patients and family caregivers manage illnesses and injuries, after her experience as caregiver for her teenage son Zachary during his 27-month battle with terminal brain cancer. Roberta realized patients and families urgently need practical, easy-to-use information and tools. Zaggo’s mission is to provide patients and families with the educational information, tools, and resources they need to become empowered, engaged, effective members of their medical teams for the best possible care. With an easy-to-use guide book and organizational tools, the ZaggoCare System is the only product to offer the comprehensive advice and tools needed to help patients and caregivers manage illness or injury. As a charitable organization, 100% of the profits from the sale of ZaggoCare are donated to innovative brain tumor research in memory of Zachary.