Last Updated on December 9, 2022
This week is National Influenza Vaccination Week in the United States. Established by the Centers for Disease Control and Prevention (CDC) in 2005, this week highlights the importance of continuing flu vaccination through the holidays and beyond. Vaccines against the flu are the best defense against the virus and developing flu-related complications.
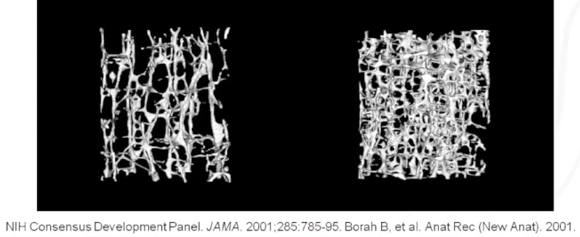
The influenza vaccine contains elements of killed or inactivated viruses. The dead virus still contains the antigens they had when active, and a person’s immune response is similar to the immune response from an infection. Despite misconceptions, the flu shot can not cause the flu. Due to the quickly-evolving nature of influenza, annual flu shots are necessary to protect against the circulating variants. No vaccine is 100% effective at preventing infection but vaccines do reduce disease severity, slow transmission, and protect vulnerable populations — including young children, elderly adults, and people with weakened immune systems and/or other chronic health conditions.
We’ve covered the similarities and differences of influenza and COVID-19 in the past. The symptoms of both are nearly identical: fever, cough, tiredness, muscle aches, sneezing, sore throat, runny/stuffy nose, nausea, diarrhea, and loss of smell/taste. The flu is generally only transmissible while symptomatic and does not pose the same risk of severe illness as COVID-19. In contrast, the novel coronavirus can spread weeks before symptoms appear and can lead to blood clots and multisystem inflammatory syndrome.
Mitigation efforts to slow the spread of COVID-19 early in the pandemic greatly affected the spread of influenza. During the 2019-2020 pre-pandemic flu season in the United States, up to 56 million people tested positive for the flu including 740,000 hospitalizations and 62,000 deaths. The following year — after months of living socially distanced, cultural acceptance of wearing masks in public, and greater awareness of the importance of hygiene — only 1,675 positive cases of influenza were detected in the U.S., including only one report of a pediatric flu death.
With growing vaccine resistance translating to fewer people getting flu shots this year and lifting mandates on social distancing and masks, this season will have much higher levels of influenza along with the risks of spikes in COVID-19. The best time to be vaccinated is before the virus begins to spread in your community. Even if you haven’t been inoculated yet, it’s not too late. The flu commonly peaks in February and can continue through May.
Coinfection of flu and COVID-19 — catching both the influenza virus and SARS-CoV-2 coronavirus at the same time — has been linked to worse outcomes. Both COVID-19 and the flu leave the body prone to developing further infections, especially if the illness is severe enough to require hospitalization. Some researchers have estimated that as many as half of all COVID-19 deaths can be attributed to mixed infections. Analysis of more than 100 studies suggests people who tested positive for both SARS-CoV-2 and a second pathogen had triple the odds of dying compared with those who had only COVID-19.
This year’s season has the added risk of respiratory syncytial virus (RSV). RSV is mainly a risk to young children, affecting 90% of children under 2 years old — but can be fatal. A new study estimates that 1 in 50 deaths of otherwise healthy children under age 5 globally is due to RSV. RSV can also be dangerous for elderly adults and people with chronic heart or lung disease and/or weakened immune systems. Coinfection of RSV and COVID-19 has been associated with longer hospital stays (and higher healthcare costs). Coinfection of RSV and influenza have been observed to cause novel interactions that make the flu more immune evasive. Coinfection of all three at once is also possible. If you have a young child with RSV or other respiratory illness, consult a pediatrician as early as possible.
While there is currently no available vaccine for RSV, the best way to avoid influenza or coronavirus is to get vaccinated. The CDC recommends everyone over the age of 6 months to get a flu vaccine every season. Children younger than 2 years old, or children with health problems such as asthma, diabetes, or other chronic conditions are at the highest risk of severe complications of the flu and should get the flu shot. The best way to protect infants under 6 months old is to surround them with people who have been vaccinated. If you are presenting any symptoms of respiratory illness, wear a mask in public spaces or around immunocompromised people in your life to reduce the risk of spread.
If you or your family is in need of care but lack the means to find affordable treatment, NeedyMeds has a database of over 18,000 free, low-cost, or sliding scale clinics across the United States and its territories. Search your ZIP code for clinics in your area to find free or low-cost medical attention and check for Immunizations under Services. You can also use Vaccines.gov to find influenza and COVID-19 vaccinations in your area. NeedyMeds lists over 100 nationwide resources for those who have been impacted by COVID-19, as well as coupons for over-the-counter flu medication. If your insurance doesn’t cover the cost of the flu shot, the NeedyMeds Drug Discount Card may help. Many pharmacies offer a discount on the flu shot and other immunizations. The free NeedyMeds Drug Discount Card can also be used by anyone to help save money on their prescribed medication not covered by insurance — even over-the-counter medicine prescribed by a doctor. The card is available physically via mail, in a printable form, or as a smartphone app for Apple and Android devices. For more help finding information, call our toll-free helpline Monday-Friday 9am-5pm Eastern Time at 1-800-503-6897.